About the author
Oommen C Kurian is Fellow, Public Health, at the Observer Research Foundation. He is a researcher trained in economics and community health at the Jawaharlal Nehru University, New Delhi. His research interests include health policy issues, among them, the use of large datasets to analyse health trends and explore workable solutions to the issues confronting the sector. He has previously worked with Oxfam India, Action Aid India, Centre for Enquiry into Health and Allied Themes (CEHAT), Office of the Commissioners of the Supreme Court (Right to Food Case), Centre for Women's Development Studies (CWDS), Centre for Social Medicine & Community Health (CSMCH), JNU, and Women's Studies Programme, JNU. He wishes to acknowledge two anonymous referees for their valuable inputs on an early draft of this paper.
“The time spent by the field worker, especially auxiliary nurse midwives, on maintaining various registers and records ranges from 20-30 percent of the total working time. This naturally cuts down the time available for field work.” – 1979, India[1]
Introduction
Health information gathering is a key component of any working health system. However, this function is weak in low and lower middle-income countries, which are perennially plagued by problems of having data that are not only poor in quality but also inadequate for properly informing health policy.[2] Data capture is often seen as an additional burden on the already scarce human resources, which further weakens implementation capacity.
In the case of India, this systemic weakness has long been identified and acknowledged by the government. The National Health Policy of 2002 recognised the dire need for systematic and scientific population health statistics.[3] Initial assessments have identified several key issues such as lack of information on non-communicable diseases and injuries, dearth of primary data on causes of death, lack of private health sector numbers, and insufficient data at the district level.[4] India’s achievements with health data remain limited, considering that it has been a pioneer among developing countries in establishing data systems: the National Sample Surveys (NSS) was initiated in 1950, and the Sample Registration System, in the 1960s.[5]
In such a fragmented landscape, government ministries are often left with no choice but to depend on different and incompatible datasets. For example, key central ministries disagreed on whether India was on-track in achieving crucial targets of the Millennium Development Goals (MDG). A case in point is MDG 5, whose target was reduction of maternal mortality ratio (MMR) by three-quarters between 1990 and 2015. While the numbers published by the health ministry (MoHFW)[6] indicated that India will achieve this goal, the Ministry of Statistics (MoSPI) was less optimistic.[7] It turned out, however, that their respective estimations were based on two separate sets of numbers.
In early 2016, around 200 countries agreed in principle on a global indicator framework as a starting point for the 2030 Agenda and the SDGs. The 17 goals and 169 targets of the SDG framework are complemented by 230 indicators, which is a five-fold jump from the MDGs’ 48 indicators. The MoSPI and NITI Aayog are in the process of integrating the SDGs into national planning processes and finalising the national indicator framework.[8]
Nevertheless, MoSPI suggests that India currently has the capacity to produce data for only 23 out of the 230 SDG indicators. According to officials, with additional investments, India can perhaps produce data for systematically tracking some 50-60 indicators. [9] For the same reason, it will be a huge challenge to identify measurable indicators for tracking national health goals aligned to the SDG goals.[10] NITI Aayog had set itself a deadline of end-2016 for finalising a set of indicators to monitor progress across national development goals.
It is widely accepted that the MDG framework of vertical goals has contributed to the current fragmented approaches to development.[11] The SDG framework tried to overcome this anomaly by introducing a broader set of goals. Tracking these goals is going to be a daunting challenge for governments, international agencies, as well as national statistical offices. To understand the huge regional, inter- and intra-state disparities better in order to remedy them, large amounts of new information will be required. Indeed, a ‘data revolution’ is needed in terms of making disaggregated data publicly available if India is aiming to achieve—or get anywhere near—the ambitious SDG targets related to health, including those on nutrition.[12] The following sections offer four recommendations to streamline and build on the existing national statistical infrastructure to facilitate such a data revolution.
Recommendation 1: Transform Civil Registration and Vital Statistics (CRVS) systems to achieve universal coverage.
A Civil Registration System (CRS) can be considered complete if it covers at least 90 percent of all live births and deaths taking place within a country or area.[13] India has made considerable improvement over the last decade in terms of its Civil Registration and Vital Statistics (CRVS) systems coverage (See Table 1). The National Population Policy 2000 had set the goal of achieving universal birth registration by the year 2010. However, the coverage is not yet enough where the data at the national level can be used to inform decision making. Still, as of 2013, there are 28 States/UTs where the coverage of birth registration is more than 90 percent, and 17 States/UTs where the coverage of death registration is more than 90 percent.[14]
| Box 1: The significance of CRVS systems for the health system Unlike other sources of vital statistics such as censuses and household surveys, the data from Civil Registration and Vital Statistics (CRVS) systems permit the production of statistics on population dynamics, health, and inequities in service delivery on a continuous basis for the country as a whole and for local administrative subdivisions. This provides more accurate information and the ‘denominator’ for assessing progress with plans across sectors for improving economic growth and reducing poverty. Accurate vital statistics and the ability to monitor and respond to causes of death and disability underpin many global targets, including new commitments to universal health coverage and tackling the global epidemic of non-communicable diseases. Information on the cause of death, when disseminated through vital statistics, can (i) improve the allocation of resources in health services; (ii) provide early insights into trends in disease prevalence so that health officials can design prevention or intervention strategies; (iii) provide more accurate estimates of maternal mortality than are available from other sources; and (iv) reveal unusual patterns of deaths by cause that point to the need for timely interventions. |
Source: http://www.who.int/healthinfo/civil_registration/WB-WHO_ScalingUp_InvestmentPlan_2015_2024.pdf & http://data2x.org/wp-content/uploads/2014/08/CRVS-Asia-and-Pacific_Knowles.pdf
The overall level of birth registration in India was 85.5 percent in 2013, and according to official sources, 17 States/UTs have achieved the target of 100-percent birth registration, as of 2013. However, there are sharp inter-state differences, and if the two most populous and poorest performing States (Bihar and Uttar Pradesh) are excluded from the analysis, the level of registration of births rises to 96.8 percent. Similarly, the level of registration of deaths was at 70.9 percent in 2013; and as of 2013, 11 States/UTs have achieved the target of 100-percent registration of deaths. Repeating the exercise and excluding Bihar and UP from the analysis, the level of registration of deaths reaches 85.2 percent. Overall, only eight States/UTs have achieved the target of 90-percent in both birth and death registrations, as of 2013.[15]
Table 1: Civil Registration and Vital Statistics (CRVS) systems coverage in India
| Children under 5 years whose birth was registered (%) |
Level of Registration of Births |
| State |
NFHS 4 2015-16 |
NFHS 3 2005-06 |
CRS 2013 |
|
Urban |
Rural |
Total |
Total |
Total |
| West Bengal |
97.3 |
96.7 |
96.9 |
75.8 |
92.8 |
| Uttarakhand |
81.8 |
74.2 |
76.7 |
38.4 |
76.6 |
| Tripura |
96.8 |
89.9 |
91.6 |
74.4 |
91.4 |
| Telengana |
89.9 |
76.5 |
82.9 |
NA |
100 |
| Tamil Nadu |
98.5 |
98.2 |
98.3 |
85.8 |
100 |
| Sikkim |
98.6 |
98.4 |
98.5 |
85.7 |
79.9 |
| Puducherry |
99.2 |
98.7 |
99 |
NA |
100 |
| Meghalaya |
89.2 |
78.4 |
79.8 |
43.3 |
100 |
| Manipur |
74.8 |
59.7 |
64.8 |
30.4 |
100 |
| Maharashtra |
95.8 |
94.6 |
95.1 |
80 |
100 |
| Madhya Pradesh |
92.2 |
78.4 |
81.9 |
29.7 |
84.1 |
| Karnataka |
95 |
94.9 |
94.9 |
58.3 |
96 |
| Haryana |
94 |
94.3 |
94.2 |
71.7 |
100 |
| Goa |
98.9 |
99 |
98.9 |
94.7 |
100 |
| Bihar |
64.5 |
60.3 |
60.7 |
5.8 |
57.4 |
| Assam |
97.4 |
93.8 |
94.2 |
43 |
97.7 |
| Andhra Pradesh |
90.1 |
79.9 |
82.7 |
NA |
98.5 |
| A & N Islands |
97.2 |
98.4 |
97.9 |
NA |
95.8 |
Source: NFHS-4 state factsheets, CRS 2013 Report
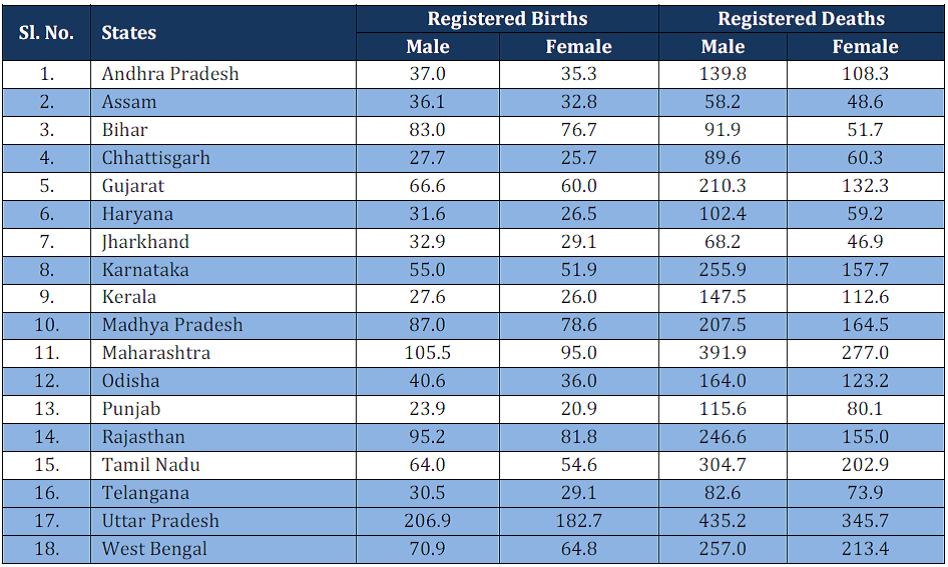
According to the latest available CRS data (2013), the share of rural areas in total infant deaths registered is only 33.1 percent. While this may suggest under-reporting in the rural areas, it could also be because deaths are registered at the place of death rather than residence. The share of overall male birth registration is 53 percent and female birth registration is 47 percent. Similarly, male deaths registered is 58 percent of total and female deaths, 42 percent, showing considerable difference.[16] State-wise figures on sex-disaggregated proportions of registered births and deaths are given in Table 2.
Table 2: Sex-wise Registered Births and Deaths of Major States (in’000), 2013
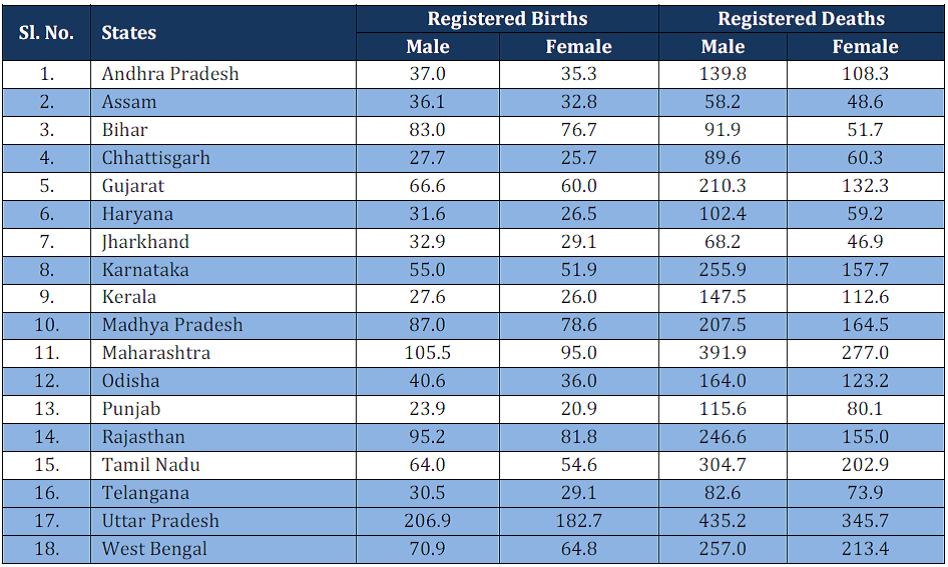
Source: http://www.censusindia.gov.in/2011-Documents/CRS_Report/CRS_Report2013.pdf
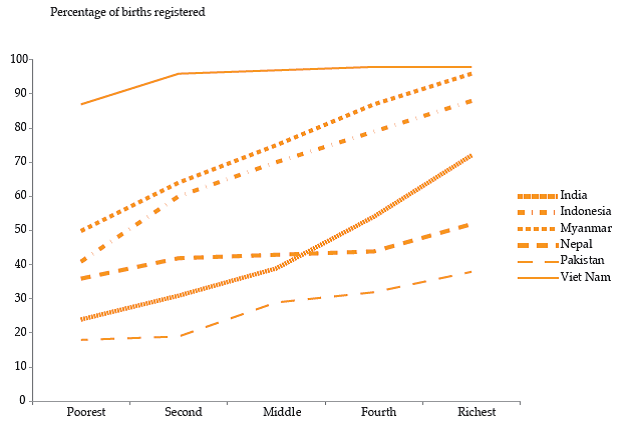
Experts emphasise that further research is needed to determine the extent to which such gender-based differentials in registration numbers represent a relatively low probability of registration for women and/or true sex differences in fertility or mortality levels themselves.[17] While previous NFHS rounds have reiterated rural-urban differences in birth registration, gender-based differences are not seen across the country, barring some states. [18] An assessment of the quality of CRS data conducted in 2014 found that Rajasthan under-registered female births. [19] Inequities based on income also remains a major constraint in achieving birth registration coverage, as Graph 1 clearly shows.
Graph 1: Birth registration of children under 5 years, by wealth quintile
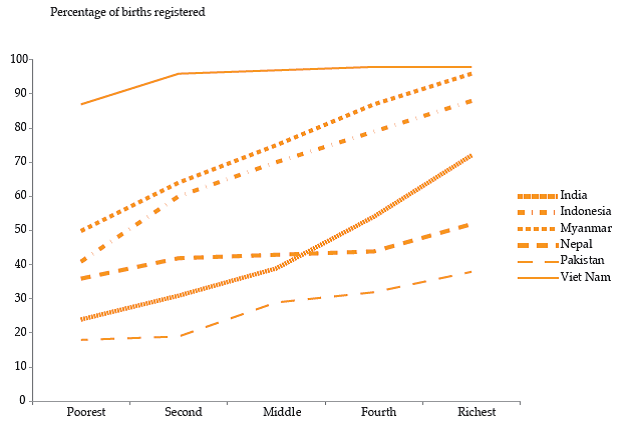
Source: http://www.unescapsdd.org/files/documents/PUB_APPJ-Vol-29-No-1.pdf
In 2014, India announced a ‘Vision 2020’ plan towards achieving universal registration of births and deaths by 2020. However, given the trends in the low-performing states, this goal appears unlikely to be achieved with the current efforts. The key strategies include dissemination of a physician’s manual for improving cause-of-death reporting. In addition, a standardised web-based software application has been developed in order to avoid different packages being used across states. [20] Another transformational initiative is the National Population Register (NPR), an electronic database of more than 1 billion residents of the country. The process of removing duplicates from the database and assigning unique identity numbers is underway. An initiative has also been launched to integrate the population register with the civil registration system. [21]
CRS has been in operation in India for a long time, and carries the legacies of the colonial rule. The diversity within the system often comes in the way of cross-coordination. A study by the United Nations Population Fund (UNFPA) in 2013 showed that as administrative systems differed considerably across India prior to independence, the timing of its introduction and the modality has also varied across space. Despite some uniformity after the introduction of the Registration of Births and Deaths Act in 1969, the actual registration is done by officials in the state governments from diverse departments. [22] Most of these officials have different primary roles, and registration of births and deaths often receives a low priority. It is observed that although interdepartmental committees exist at the state level, they are often ineffectual, adversely affecting the completeness and quality of the CRVS system. [23]
| Box 2: Who registers births and deaths in India? The Chief Registrars of births and deaths in 19 States and two UTs are from the Health Department; in 10 States and two UTs are from the Planning, Economics & Statistics Department; in one State (Kerala), from the Panchyat Department; and in the remaining two UTs, with the Local Administration and Revenue Department. The district-level authorities are mainly divided among District Collectors/District Magistrate (in nine States and one UT); Chief Medical Officers/District Medical and Health (11 States and two UT); District Statistical/ Planning Officers (in four States and one UT); and Deputy Director/Assistant Director (Panchayat) in one State and one UT; and others in remaining States/UT. At the Rural level, the registration work is entrusted to the officials of Panchayat Department in 15 States and three UTs; Health Department in seven States and four UTs; Revenue Department in three States; Education Department in two States and Police Department in one State and one UT. |
Source: http://www.censusindia.gov.in/2011-Documents/CRS_Report/CRS_Report2013.pdf
The Sample Registration System (SRS), which provided mortality statistics for national and state-level MDG tracking was introduced in the 1960s to overcome the deficiencies of the CRS. Over the years, the SRS expanded substantially, and by 2013 it covered a population of about 7.5 million.[24] It has piloted verbal autopsy procedures and reported national summaries of causes of death as part of the Million Deaths Study,[25] which, in turn, have produced morbidity burden estimates far greater than previously believed. This system is not without its shortcomings, though. For example, a recent study based on SRS found that in Rajasthan, 27 percent of female deaths were being missed, suggesting underreporting.[26] The CRS system collects limited data on socio-economic status, and SRS does not collect it at all. Moreover, unit-level records of SRS are not made available for researchers. [27]
However, the current focus on entrenched interim measures like SRS cannot take away from the need for universalisation of civil registration through adequate “legal, budgetary, and administrative support”.[28] Expansion of the CRS system, including collection of socio-economic data of the deceased remains the single most important goal for improving India’s health statistics infrastructure. Emphasis needs to be put on Bihar and Uttar Pradesh, which considerably pull down the national average for coverage. Steps are needed to improve the quality of data on causes of death collected through verbal autopsy. Fragmentation in the system needs to be overcome, and there must be interdepartmental coordination at the state level. Further, options should be explored to collect data on socioeconomic background as part of SRS and enhance the sample to produce district-level estimates across socio-economic categories.
In 2011 the Commission on Information and Accountability for Women's and Children's Health, led by the World Health Organization (WHO), had made 10 recommendations around timely, reliable and accessible health information and data.[29] India was one of the six countries in the South-East Asian region of WHO to make a commitment to implement the 10 recommendations of the Commission. By 2014, eight of the 11 countries in the region had conducted comprehensive assessments of their CRVS systems.[30] However, WHO still has to succeed in pushing the Government of India to conduct the CRVS assessment at the earliest.[31]
Recommendation 2: Streamline existing national surveys in a way that will improve disaggregated tracking of national goals.
Given the incomplete coverage of CRVS, large-scale, population-based household surveys play an invaluable role in providing health and nutrition information in India.[32] Reviews have shown that population-based surveys are used extensively to gather information on fertility, mortality, family planning, maternal and child health, and some other aspects of health, nutrition and healthcare in India.[33]
The latest round of the National Family Health Survey (NFHS 2015-16), for the first time in its history, gives district-level estimates. NFHS will now repeat every three years according to plans, and will no doubt help overcome some of India’s health and nutrition data bottlenecks. NFHS 4 replaces the annual health survey (AHS) and district-level household and facility survey (DLHS) – two major sources of health data at the district level during the MDG era.[34] However, as DLHS is the only database so far which has health system-level variables, village-level characteristics and household characteristics, an appraisal may be necessary to determine how such gap would be filled, in the absence of DLHS. The unavailability of regular, good-quality data remains a constraint in the country’s health and nutrition policy. This has an impact on the nature of policy discussions as well, which often remain an exchange of polarised views, uninformed by numbers.
The National Sample Survey (NSS)—set up in 1950 to bridge the large gaps in statistical data needed for planning and policy formulation—still does not give reliable district-level estimates for most indicators. Health-related data that are collected by NSS through what is commonly known as ‘central sample’ data, are a major source for policy research in the country. [35] Many experts fear that over the last two decades, developments like cuts in staff strength, change in recruitment practices, and the creation of a ‘centralised’ Subordinate Statistical Service have resulted in a shortfall of experienced field investigators, which may have compromised the quality of data being collected by the NSSO.[36] The data are regularly analysed and put in the public domain by MoSPI, and unit-level data made available for a fee. However, considerable resources are also spent to collect what is known as the ‘state sample’, which covers at least a matching number of respondents in each state. Pooling of central and state samples will enhance the policy relevance of NSS data, as these can then be used to arrive at district-level estimates. There have been discussions around pooling of NSS data, though nothing concrete has happened around the idea.[37]
Data availability for major determinants of health like nutrition is severely limited, too. A review of sources of nutrition data in India conducted by the International Food Policy Research Institute (IFPRI) in 2015 identified serious data gaps.[38] One of the major areas of action identified by the exercise was to prioritise nutrition as a development indicator. It also recommended the establishment of a reliable system for periodic data-driven updates on the state of nutrition in India. Meanwhile, the Global Nutrition Report’s India country profile highlighted significant gaps including that of timeliness of data.[39] Time series data are not available for core indicators and comparability remains a major challenge, as reference group inconsistencies in child anthropometry within surveys- affects the flexibility of analysis. NFHS, for example, had looked at children under the ages of 4, 3 and 5 for round 1, 2 and 3 respectively. With the National Nutrition Monitoring Bureau (NNMB) having been shut down in 2015, there is a need to take concrete steps towards nutrition monitoring; the NNNB was a major source of data on dietary intake and nutritional status.[40]
In this context, modifying existing surveys in terms of the data collected and their frequency is a policy imperative if India is to have a comprehensive set of health and nutrition indicators to continuously track its health and nutrition targets. Some new variables will need to be tracked. For example, household food insecurity (HFI), a key determinant of stunting in poor Indian children, is not routinely measured by large-scale demographic surveys.[41] A Food Insecurity Experience Scale (FIES) is now being piloted in the Comprehensive National Nutrition Survey (CNNS) conducted by UNICEF and the Ministry of Health and Family Welfare.[42] After testing for the scale’s validity and reliability, it can be added to national surveys to effectively track food security.
At present, in the NSS rounds dealing with social consumption of health, households as well as people are segregated in terms of location—urban or rural—according to their place of domicile, and not by the place where they sought treatment. [43] If an extra question on the location of the institution where healthcare is sought is added to the survey instrument, it will considerably expand the scope of analysis. For both NSS and NFHS rounds, more information on communicable diseases as well as non-communicable diseases (NCDs) will need to be collected. After all, India’s States are at various stages of development and, moreover, at different stages of demographic and epidemiological transition. Effective management of India’s double burden of communicable diseases and NCDs will require a regular supply of reliable data that can be disaggregated at the district level, or even lower. Since the government’s health management information system (HMIS) is currently limited in its scope, there is a need to strengthen regular surveys to give more timely information on the country’s disease burden—which is undergoing a transformation. As a starting point, an assessment on the spread and quality of information on communicable and non- communicable diseases burden available in our large surveys needs to be conducted.
In addition, an evaluation of survey modules and removal of some questions from survey tools that do not give reliable data can be considered. The module in the NSSO health round dealing with particulars of pre-natal and post-natal care for women is a case in point. There is general agreement that as alternative sources like NFHS dealing with mothers of the same age-group (15-49 years) providing data of better quality are available, the data collected by NSSO on this aspect is not being optimally used.[44]
There is a need to combine the consumer expenditure rounds with at least some modules of the social consumption of health rounds so that enhanced data is collected at more regular intervals. Centralised efforts in pooling state and central samples of NSS data needs to be made, as unused state samples across the decades involve unacceptable levels of financial wastage. When pooled, NSS rounds can offer reliable, district-level estimates for most variables, and this can help more localised planning and course correction.
The latest survey rounds have proven that India has made much headway in terms of physical access. However, financial protection remains a major concern. The NSS 71st round shows that it is the poorest quintile, for example, that has the highest rate of increase in out-of-pocket health spending in real terms. [45] Affordability and quality needs to be explored by the surveys in a more systematic manner.
Further, compatibility between the different health surveys needs to be brought about. For example, while NFHS-4 collected information separately about different types of government funded insurance schemes, NSS 71st round merged into a single variable, all government funded insurance schemes such as the Employees State Insurance Scheme (ESIS), Central Government Health Scheme (CGHS), Rashtriya Swasthya Bima Yojana (RSBY), Arogyasri, and other programmes focusing on BPL populations. This has limited the scope of analysis, particularly of the schemes meant to help the poor.
Robust policy documents raising precise questions are required, and data will need to be collected based on these, avoiding duplication and redundancy. A yearly survey covering all major indicators of health and nutrition by NSSO should be considered, after a need assessment effort mapping all the available surveys to assess adequacy of data to measure progress across national development goals in health and nutrition.
Lastly, given the fact that district-level estimates are possible with NSS (with pooling of state and central samples) and NFHS (Round 4 onwards), it is imperative to explore ways whereby survey instruments are tweaked to make it possible to conduct analysis at the level of parliamentary constituency. Perhaps, after making adjustments in the sample, adding a single question on the parliamentary constituency (NSS and NFHS) to make basic constituency-level analysis possible, will contribute to pushing health and nutrition into the arena of election debates.
Recommendation 3: Reform the national Health Management Information System (HMIS)
The Manual on Health Statistics in India (2015), published by the Ministry of Statistics and Programme Implementation, lists multiple benefits that can be reaped from higher investments in HMIS. They include the following: “helping decision makers to detect and control emerging and endemic health problems, monitor progress towards health goals, and promote equity; empowering individuals and communities with timely and understandable health related information, and drive improvements in quality of services; strengthening the evidence base for effective health policies, permitting evaluation of scale-up efforts, and enabling innovation through research and; improving governance, mobilizing new resources and ensuring accountability in the way they are used”. [46] An efficient national health information system facilitates transparent and evidence-based decisionmaking which, in turn, leads to improvements in health outcomes.[47]
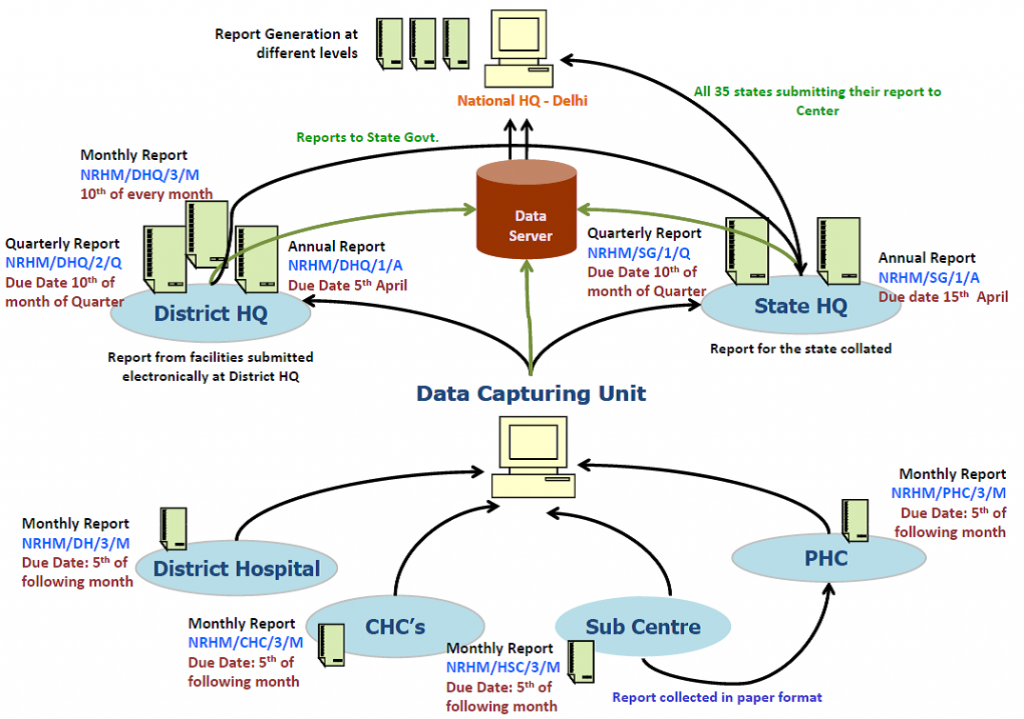
India launched the `National Rural Health Mission' in 2005, which was later renamed `National Health Mission' (NHM) in 2013 with the addition of the `National Urban Health Mission' . HMIS was intended as a management information system to oversee the working of the mission. As part of NHM, approximately 1.8 lakh health facilities capture data for HMIS about antenatal coverage, immunisation coverage, delivery services, family planning coverage indicators, among other variables.[48] Graph 2 shows the data flow within the HMIS.
Graph 2: Data Flow within National HMIS
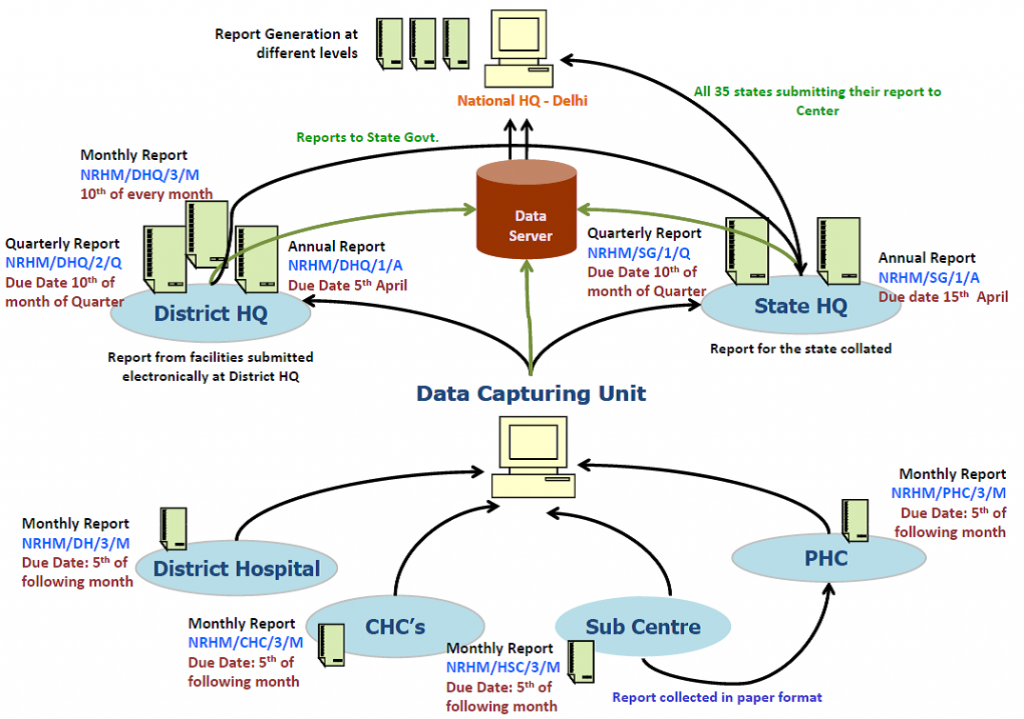
Source: http://www.abtassociates.com/AbtAssociates/files/99/994803a2-bcef-4b96-8a2b-3900e879b188.PDF[/caption]
Under-reporting of deaths of mothers and infants in the Health Management Information System (HMIS) is covered often in the media.[49] However, the weaknesses of HMIS are well-researched and acknowledged by the government itself. Studies have suggested rationalisation of registers and reports by discarding those with poor managerial value and amalgamating those with duplication, thus saving resources and easing staff burden.[50] Apart from under-reporting of deaths and lack of coverage of private sector, the HMIS system does not provide information on the exposed population, thus making it impossible to calculate different indicators.[51]
The latest annual report of HMIS (2014-15) admits that it covers only 12.7 percent of the annual estimated infant deaths and 24.8 percent of the annual estimated maternal deaths. At the same time, due to under-reporting of births and reporting of immunisation on the same child by more than one facility, the percentage of fully immunised children in India is shown consistently above 100 percent. The latest NFHS round, however, shows that immunisation coverage is much lower.[52] To inform evidence-based decision making, HMIS in India will have to improve tremendously, with a focus on integration of existing infrastructure like the Integrated Disease Surveillance Programme (IDSP) and on collection of data from the private sector.
Keeping in mind its potential and limitations as a tool to measure India’s progress in health and nutrition, an assessment of various Management Information Systems (Table 3) should be conducted. This should be done with the aim of developing a comprehensive platform like District Information System on Education (DISE), providing information on public as well as private sector. To track progress across national development goals (health and nutrition) in an integrated manner, the role of the following initiatives should be clarified, and modalities of data sharing must be developed.
| Table 3: Government Initiatives |
| § Integrated Health Information Platform (IHIP) § Health Information Exchange (HIE) § Mother and Child Tracking System (MCTS) § ICT enabled Real Time Monitoring (ICT-RTM) of ICDS § Common Application Software (ICDS-CAS) § Health Management Information System (HMIS) of NHM § National Vector Borne Disease Control Programme (NVBDCP) § Integrated Disease Surveillance Programme(IDSP) § National Programme For Prevention and Control of Cancer, Diabetes, Cardiovascular Disease and Stroke(NPCDCS) § National Program for Control of Blindness § NIKSHAY- A web based solution for monitoring of TB patients § State level initiatives like `Maternal Infant Death Review System' (MIDRS) and Anaemia Tracking System (ATM) of Haryana |
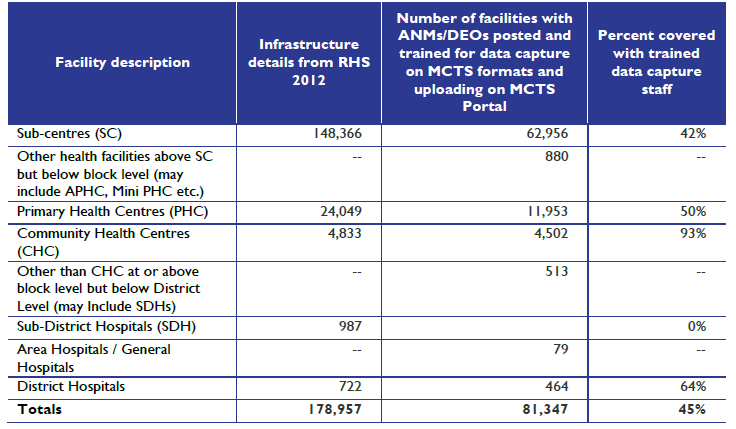
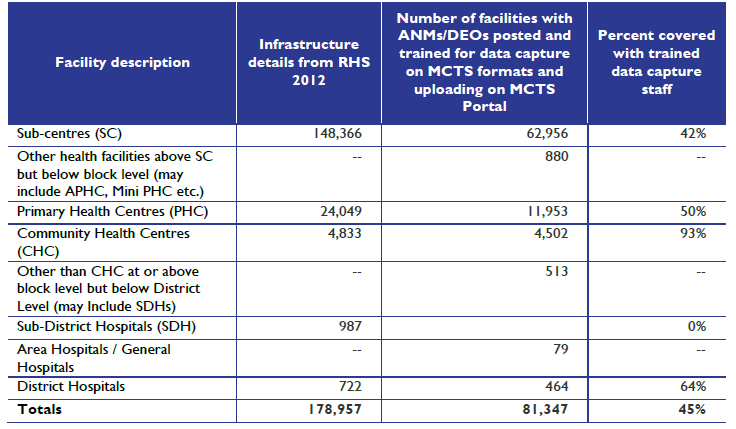
However, coverage of health facilities with trained data reporting staff presents an additional challenge as personnel shortages continue to be a crucial constraint in India’s public healthcare delivery system. A study conducted in 2014 by USAID assessed that only 45 percent of public healthcare delivery facilities in India had trained data capture staff (Table 4). Latest research from Haryana shows that HMIS records for RMNC services at sub-centre level in the state were satisfactory in terms of completeness. At the same time, there were quality concerns in the form of significant differences in terms of reported and evaluated coverage of services. The authors conclude that the quality of HMIS needs to be improved to make it relevant for public health programme planning and research.[53]Often, multiplicity of initiatives prevents a holistic health systems approach, leads to duplication and redundancies, and makes coordinated delivery difficult as observed in the 12th Plan document. Various initiatives announced by the Health as well as the Women and Child Development ministries can be mapped in a way that there is a comprehensive set of indicators aiding in both the assessment of the system and the tracking of progress. This should be followed by efforts in consolidation and rationalisation of existing systems.
Table 4: Approximation of NRHM Health Facilities with Trained Data Capture Staff
Source: http://www.abtassociates.com/AbtAssociates/files/99/994803a2-bcef-4b96-8a2b-3900e879b188.PDF[/caption]
The large government-funded health insurance schemes can be used as a means to hasten the progress in regulation of private medical institutions and to ensure a regular flow of information from the private sector, which remains a blind spot even in the case of notifiable diseases.[54] Researchers are of the view that it might take time for the HMIS to stabilise and provide quality data that will prove useful in understanding the magnitude and trend of inequality in service utilisation across time, space, and population subgroups.[55] However, a highly efficient HMIS is indispensable for any functional public health system. Tamil Nadu’s transition in 10 years into what is being called a ‘paperless health system’[56] and what Punjab is trying to achieve (Box 3) can offer some policy insights. The launch of the GIS-enabled HMIS application in May 2016 was a step in the right direction.[57]
| Box 3: Integrated HMIS of Punjab: A work in progress Fragmentation is a major problem faced by Health Information Systems in most states, and are typically saddled with historically institutionalised ‘vertical’ programs, each collecting their individual information independent of other programs, with little regard to supporting the overall information systems within the state. The result of this is excessive data, with great overlaps of the same data collected many times, and sometimes leaving large gaps in critical areas with no data at all. This is also aggravated by data and indicators being poorly standardised and represented in incompatible formats, making comparisons and analysis across program areas, difficult. To overcome this fragmentation, Department of Health & Family Welfare, Punjab, has initiated the process of integration of information systems across all health programmes. The purpose of this integration is to enable a seamless flow of data from different sources available at ‘one point’. This will give a more holistic overview of health system performance, to facilitate discussions of evidence-based planning and initiating the use of information for action. |
Source: http://pbhealth.gov.in/hmis_portal.html
Recommendation 4: Set Up a National Forum on Health and Nutrition Statistics
If India is aiming to improve the quality, availability and timeliness of data necessary to track national health goals, it has to address the core issue of fragmentation of efforts. Routine monitoring systems of the flagship schemes may not be attuned to provide reliable data. Although several government departments and ministries collect data across institutions and other stakeholders, these are not in line with standard definitions.[58] This calls for systematic efforts at the national level, taking state governments and departments on board.
Further, there is a need for an institutional mechanism to coordinate efforts in improving health and nutrition statistics in the country (Forum on Health and Nutrition Statistics).[59] The Forum on Child and Family Statistics of the US can offer important policy lessons in this endeavour. This mechanism will be a collection of various Central government agencies and ministries which are currently custodians of different sets of health and nutrition data. The mission of the Forum should be to foster coordination and collaboration and to enhance consistency in the collection and reporting of health and nutrition data. [60] To start with, this strategy must involve the Ministry of Home Affairs (office of the census commissioner and registrar general), Ministry of Statistics and Programme Implementation, Ministry of Health and Family Welfare (NFHS, HMIS, IHIP, MCTS, HIE), Ministry of Women and Child Development (ICT-RTM, ICDS-CAS) and the NITI Aayog, along with state-level functionaries.
It is often noted that India’s existing database on health workers remains inadequate, with information on those employed in public sector health facilities but no information on the large numbers in private practice. Professional registries are of limited use, as they do not reflect retirement, death or migration of health professionals. [61] In this context, the Census remains an underutilised resource. In 2016, WHO published the first definitive report on state-level health workforce in India – only that it is based on Census 2001 data. Having such a long 15-year lag, its policy relevance is highly limited, other than to function as a useful baseline.[62] An immediate objective of the Forum should be to conduct a comprehensive study on the health workforce in India, analysing the latest Census data, to inform policies on medical education based on decadal trends.
Moreover, the Forum should standardise definitions, streamline collection of data, triangulate existing data, and avoid duplication in order to bring out a comprehensive set of indicators every year which will track health and nutrition progress across the country at the sub-district level, across different attributes. Policy lessons can be derived from what the India HIV/AIDS Resource Centre has undertaken in terms of triangulation of data--analysing data from behavioural studies, epidemiological studies, and other health system datasets to arrive at a district situational analysis.[63] The Forum should take up initiatives such as pooling of NSS central and state samples so that currently under-utilised NSS datasets are of use to policymakers, academics, researchers and frontline workers.
If gaps still remain in terms of data elements needed to track national health and nutrition targets at the district level , the Forum should facilitate an annual technology-driven survey providing panel data across particularly badly performing parliamentary constituencies/districts, as an interim measure.
Panellists:
Prof Bibek Debroy, Member, NITI Aayog
Dr Krishna Kumar, DDG, MoSPI
Mr Sunil Nandraj, Advisor (Clinical Establishment Act), MoHFW
Ms Anjali Nayyar, Senior Vice President, Global Health Strategies, India
Mr Ashok Malik, Distinguished Fellow, ORF
Dr Charu C. Garg, Advisor, NHSRC
Dr Karanvir Singh, Member, MoHFW/FICCI Committee and CMIO, Apollo Hospital
Prof P. M. Kulkarni, Former Professor, JNU
Ms Priyanka Saksena, Technical Officer, World Health Organisation
Ms Ratna Anjan Jena, Advisor, WCD
Dr Vikrom Mathur, Senior Fellow, ORF
Endnotes
[1] V.S Badari., et al. Management information and evaluation system for health and family welfare programmes in rural areas. (Bangalore, India: Population Centre, India Population Project, 1979).
[2] Rakhi Dandona, et al. “A review of national health surveys in India.” Bulletin of the World Health Organization, 94 (2016): 286-296. Accessed at http://www.who.int/bulletin/volumes/94/4/15-158493/en/
[3] Magdalena Z Raban, et al. “Essential health information available for India in the public domain on the internet.” BMC Public Health 9, no. 1 (2009): 208. Accessed at http://bmcpublichealth. biomedcentral. com/articles /10.1186/1471-2458-9-208
[4] Ibid
[5] F. Ram, et al. Human Development: Strengthening District Level Vital Statistics in India. ( Mumbai: IIPS,2005). Accessed at http://iipsindia.org/publications05_b_09c.htm
[6] Press Information Bureau, Ministry of Health and Family Welfare. “Steps Taken to Reduce IMR and MMR.” Government of India (2015). Accessed at http://pib.nic.in/newsite/PrintRelease.aspx?relid=116061
[7] Ministry of Statistics and Programme Implementation (MOSPI). “Millennium Development Goals India Country Report”. (New Delhi: MOSPI, Government of India, 2015). Accessed at http://mospi.nic.in/Mospi_ New/upload/mdg_26feb15.pdf
[8] Oommen C Kurian, “Can a Data Revolution Help India Achieve Its Health Goals?” The Wire. (2016). Accessed at http://thewire.in/48429/data-india-health-nutrition-sustainable-development-goals/
[9] Rhea Colaco. “Developing an Indian approach to SDG indicators in health and nutrition.” Observer Research Foundation. (2016). Accessed at https://orf.di91.com/research/developing-an-indian-approach-to-sdg-indicators-in-health-and-nutrition/
[10] Tanoubi Ngangom, “Building a Follow-up and Review Framework for India's Sustainable Development Goal on Health” ORF Issue Brief No 155, Observer Research Foundation, New Delhi, 2016.
[11] Ilona Kickbusch and Callum Brindley. Health in the Post-2015 Development Agenda. (Geneva: World Health Organization, 2013).
[12] Oommen C Kurian, Op cit.
[13] Registrar General. “Vital Statistics of India Based on the Civil Registration System 2013.” Office of the Registrar General of India, Ministry of Home Affairs, New Delhi (2015), Accessed at http://www.censusindia.gov.in/2011-Documents/CRS_Report/CRS_Report2013.pdf
[14] Ibid
[15] Ibid
[16] Ibid
[17] Mamta Gupta, et al. “Estimating mortality using data from civil registration: a cross-sectional study in India.” Bulletin of the World Health Organization, 94 (2016): 10-21. Accessed at http://www.who.int/bulletin/volumes/94/1/15-153585/en
[18] International Institute for Population Sciences (IIPS) and Macro International.National Family Health Survey (NFHS-3), 2005–06: India: Volume I.( Mumbai: IIPS, 2007).
[19] Institute for Social and Economic Change (ISEC), Centre for the Study of Regional Development and United Nations Population Fund. A Preliminary Assessment of the Quality of Civil Registration System in Kerala, Odisha and Rajasthan. (Bangalore: ISEC, 2013).
[20] United Nations Economic and Social Commission for Asia and the Pacific. Asia-Pacific Population Journal, Vol. 29, No. 1 (2014).
[21] Ibid
[22] Institute for Social and Economic Change (ISEC), et al, Op cit.
[23] United Nations Economic and Social Commission for Asia and the Pacific, Op cit.
[24] Nandita Saikia and P.M. Kulkarni. “Data for Research into Health Inequality in India.” The Economic and Political Weekly 51, 26 and 27 (2016): 111-116.
[25] Mamta Gupta, et al. Op cit.
[26], Ajit Yadav “Measurements and Challenges of Adult Deaths Completeness in India and Selected States: An Analytical Study of Different Methodologies.” Population Association of America 2015 Annual Meeting, San Diego, April 30, 2015.
[27] Charu C. Garg. Availability, Quality and Data Gaps in Health Statistics in India. (Ministry of Statistics and
Programme Implementation: Government of India, 2014).
[28] Nandita Saikia, and P.M. Kulkarni. Op cit.
[29] Commission on Information and Accountability for Women's and Children's Health. Recommendations. (World Health Organisation. Geneva. Undated) Accessed at http://www.who.int/woman _child_ accountability/ about/coia/en/index5.html
[30] WHO Regional Office for South-East Asia. Covering every birth and death: Improving civil registration and vital statistics (CRVS). (New Delhi: WHO. 2014) Accessed at http://apps.searo.who.int/PDS_DOCS/B5150.pdf
[31] WHO Regional Office for South-East Asia. Health situation and trend assessment. (New Delhi: WHO. Undated) Accessed at http://www.searo.who.int/entity/health_situation_trends/topics/crvs/en/index1.html
[32] Prashant Kumar, “Tracking Hunger and Nutrition SDG Targets: Gaps, Challenges and Possibilities” ORF Issue Brief No 149, Observer Research Foundation, New Delhi, ( 2016)
[33] Rakhi Dandona, et al, Op cit.
[34] Oommen C Kurian, Op cit.
[35] Conference of Central and State Statistical Organisations (COCSSO). State Sample Data of National Sample Surveys Status of Processing and its Relevance in the Context of Pooling. ( New Delhi:COCSSO, Ministry of Statistics and Programme Implementation. 2015).
[36] Sheila Bhalla, “Behind the Post-1991 ‘Challenge’ to the Functional Efficiency of Established Statistical Institutions”, Economic and Political Weekly, Vol. 49, Issue No. 7. (2014).
[37] Oommen C Kurian, Op cit.
[38] Aparna John, et al. “An assessment of data sources to track progress toward global nutrition targets in India.” POSHAN Research Note 6, International Food Policy Research Institute (2015). Accessed at http://ebrary.ifpri.org/cdm/ref/collection/p15738coll2/id/129722
[39] “Nutrition Country Profiles.” Global Nutrition Report, International Food Policy Research Institute (2015). Accessed at http://globalnutritionreport.org/the-data/nutrition-country-profiles/
[40] Vidya Krishnan, “Nutrition bureau axed, anti-poverty schemes starved.” The Hindu, (2015), Accessed at http://www.thehindu.com/news/national/national-nutrition-monitoring-bureau-axed-antipoverty-schemes-starved/article7815511.ece
[41] V Sethi, et al, ‘Usage, internal validity and reliability of experience-based household food insecurity scales in Indian settings’, Nutrition Reports, issue 5, United Nations Children’s Fund, New Delhi, India, (2016).
[42] Ibid.
[43] National Sample Survey Office. Social Consumption: Health, NSS 71st Round : Jan - June 2014.( New Delhi: Ministry of Statistics & Programme Implementation, Government of India2015). Accessed at http://mail.mospi.gov.in/index.php/catalog/161
[44] Ministry of Health & Family Welfare. "Key Findings from NSSO Surveys Related to Health." Workshop, Ministry of Health & Family Welfare, New Delhi, August 3-4 (2016)
[45] Shamika Ravi, Presentation at "Key Findings from NSSO Surveys Related to Health." Workshop, Ministry of Health & Family Welfare, New Delhi, August 3-4 (2016).
[46] Central Statistical Office. Manual on Health Statistics in India. (New Delhi: Ministry of Statistics & Programme Implementation, Government of India. 2015), Accessed at http://mospi.nic.in/mospi_new/upload/Manual-Health-Statistics_5june15.pdf
[47] Michael P Rodriguez, et al. Synthesis Report of Health Information Systems in India. Health Finance & Governance Project, (Bethesda, MD: Abt Associates Inc. 2014).
[48] Smriti Sharma, “Problems of the Health Management Information System (HMIS): the experience of Haryana.” Ajay Shah’s blog (2016). Accessed at https://ajayshahblog.blogspot.in/2016/06/problems-of-health-management.html
[49] Sushil Manav, “Haryana districts ‘hide’ mother-infant deaths.” The Tribune (2015) , Accessed at http://www.tribuneindia.com/news/haryana/governance/haryana-districts-hide-mother-infant-deaths/114117.html
[50] UM Bhojani, et al. “Under reported deaths and inflated deliveries: making sense of health management information systems in India.” International Conference on Health Systems Strengthening, Chennai, ( 2010).
[51] Nandita Saikia and P.M. Kulkarni. Op cit.
[52] Vandana Prasad and Indranil Mukhopadhyay. “India's wealthier states are showing an alarming decline in immunisation rates.” Scroll. (2016) Accessed at http://scroll.in/pulse/812221/indias-wealthier-states-are-showing-an-alarming-decline-in-immunisation-rates
[53] Atul Sharma, et al. “Quality of Health Management Information
System for Maternal & Child Health Care in Haryana State, India”, PLoS ONE 11(2), (2016)
[54] Rhea Colaco, Op cit.
[55] Nandita Saikia and P.M. Kulkarni, Op cit.
[56] Ramesh Govindaraj. “How the Tamil Nadu Health System was transformed to a paperless health system in just 10 years” World Bank Blogs, (2016).
[57] Press Information Bureau. “ Shri J P Nadda launches GIS-enabled HMIS application, self-printing of e-CGHS Card”, Government of India. 2016. Accessed At http://pib.nic.in/newsite/PrintRelease.aspx?relid=138397
[58] Registrar General of India. “Agenda-3: Statistics on Children.” Ministry of Health & Family Welfare, (2008) Accessed at http://mospi.nic.in/Mospi_New/upload/15_agenda/Agenda-3_280108.pdf
[59] A similar recommendation was made by UNICEF India to MoSPI ion 2008, focusing on monitoring outcomes for children in India. Available at Registrar General of India. “Agenda-3: Statistics on Children.” Ministry of Health & Family Welfare, (2008) http://mospi.nic.in/Mospi_New/upload/15_agenda/Agenda-3_280108.pdf
[60] “Agenda-3: Statistics on Children.” Ministry of Health & Family Welfare, (2008), Accessed at http://mospi.nic.in/Mospi_New/upload/15_agenda/Agenda-3_280108.pdf
[61] Sudhir Anand and Victoria Fan. “The Health Workforce in India.” Human Resources for Health Observer Series No. 16, Geneva: World Health Organization, (2016).
[62] Ibid
[63] Available at http://indiahivinfo.naco.gov.in/naco/tags/data-triangulation
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

 PDF Download
PDF Download



 PREV
PREV