Introduction
Infertility, defined by the World Health Organization (WHO) as failure to achieve pregnancy after 12 months of regular unprotected sexual intercourse,[1],[2] affects an estimated one in every six people globally.[3] Female fertility declines with age, particularly after 30, and accelerates after 35.[4] Age is also associated with diminished semen volume and sperm motility in men.[5] Infertility is classified as either primary (never conceived) or secondary (at least one prior pregnancy) and arises from various factors. Female infertility can be attributed to endocrine, ovarian, uterine, or tubal disorders; male infertility, meanwhile, can result from obstructive disorders, endocrine/hormonal imbalances, testicular dysfunction, or sperm function and quality issues.[6] While the causes vary across countrie,[7] infertility typically carries social stigma across cultures, adding to the emotional burden faced by those who experience it.
Infertility impacts sexual and reproductive health and rights, affecting the well-being of married couples. The ability to decide the number, timing, and spacing of children is a key indicator of both physical and mental health.[8] WHO, recognising regional variations in the primary causes of infertility—such as infections being more prevalent in Asia and Africa, and tubal and endocrine factors in developed nations[9]—has prioritised prevention and early detection. Recognising infertility as a public health issue, countries are taking steps to mitigate the challenge. For example, the United States has a national action plan for infertility, Moldova has included infertility prevention and management in its national health plan, and Malawi aims to reduce infertility rates under its national reproductive health policy. A 2017 study showed that nine European countries have laws providing access to infertility treatments.[10]
While India has made progress in addressing infertility, its focus remains primarily within the private sector, largely serving married couples. The Assisted Reproductive Technology (ART) Bill, 2021, regulates ART clinics and banks, establishing a code of conduct and standards for service providers while addressing the rights of those seeking ART services and those of children born with the assistance of these technologies. However, preventive measures remain largely absent from the Indian health system.[11],[12] Community-based approaches, which proactively involve local populations in research and intervention design, have demonstrated positive results in addressing health disparities and improving healthcare access.[13] Such approaches offer a promising opportunity for enhancing infertility prevention and care.
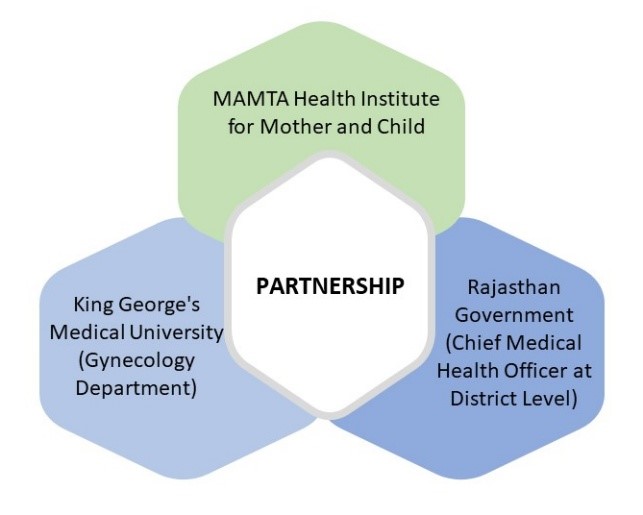
Figure 1. Rationale
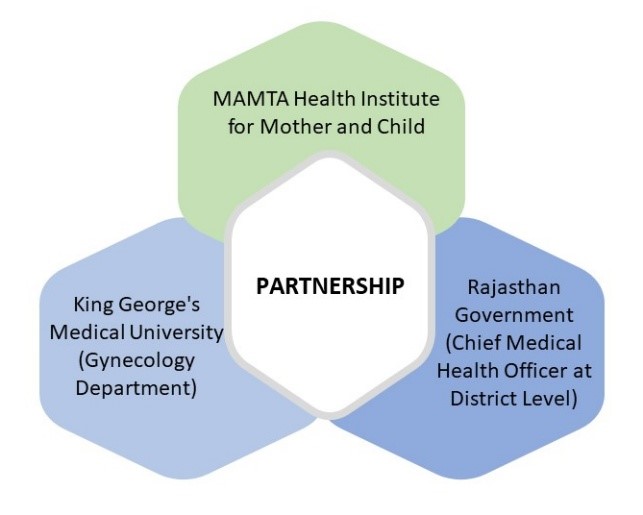
Source: Authors’ own
Investigating the prevalence of infertility is crucial for developing effective prevention and early detection strategies tailored to regional needs. Understanding community experiences around infertility provides essential data for resource allocation, programme development, and targeted interventions.
In 2023, the Rajasthan government, in partnership with MAMTA-HIMC and the Infertility and IVF Unit at Queen Mary’s Hospital, Lucknow, conducted an infertility prevalence investigation to address the information gap at the community level. The study covered 156 villages, selected based on recommendations from the block government, which prioritised areas with limited access to reproductive health services for the survey from Kotkasim and Tijara blocks of Alwar. A trained data collection team aimed to gather evidence-based insights to estimate infertility prevalence and identify potential risk factors.
Methodology
Survey Participants
The survey covered married women ages 18 to 49, residing in the selected 156 villages of Kotkasim and Tijara blocks, who are yet to experience menopause and have not undergone hysterectomy. A total of 26,360 women were surveyed, all meeting the inclusion criteria and eligible to participate.
Inclusion criteria:
- Married couples ages 18–49 years.
- Couples residing in the project area for at least a year.
- Couples consenting to participate in the survey.
Subsequently, qualitative interviews were conducted with personnel in charge (chief health officer/ANM). Data collection was conducted by a team of five trained data collectors, who received two days of in-person training from qualitative and quantitative researchers.
Sampling Methodology
As per the population distribution, the villages were sorted in ascending order at three levels (top, middle, and lower). The top five villages were selected from the population-wise segregated list, resulting in a total of 15 villages. The sample was drawn randomly from the list of eligible couples.
The formula used for the calculation of the sample size is mentioned below.
n= z2 P (1-P)/d2
Where,
n = sample size
Z = statistic corresponding to the level of confidence
P = expected prevalence
d = precision
P = The prevalence of the women whose Body Mass Index (BMI) is below normal (BMI<18.5Kg/m2) is (21.3 percent)[a]
For this study, among the prevalence of all the primary objectives, the nutritional status of women ages 15-49, women whose Body Mass Index (BMI) is below normal (BMI<18.5Kg/m2) was 21 percent had the lowest prevalence.
Z = 1.96 confidence interval (at 95 percent)
d = absolute error of 5 percent
After adjusting for the non-response rate of 20 percent, the final sample size turned out to be 339.
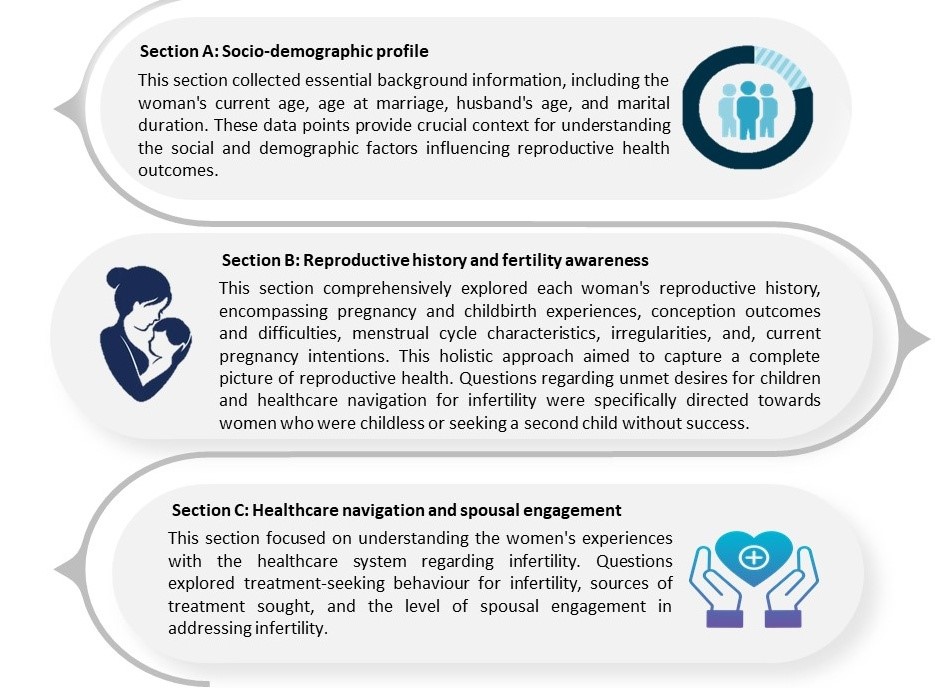
The Survey Tool
The survey tool is a structured questionnaire designed to capture women's reproductive histories, and was developed in collaboration with the Infertility and IVF Unit (Obstetrics and Gynaecology) at Queen Mary’s Hospital. The questionnaire was divided into three sections to facilitate systematic data collection and analysis. This structured format enhanced the rigour and reliability of the research findings, allowing field researchers to navigate the instrument efficiently and accurately.
Ethical Approval
Ethical approval was obtained from the Institutional Review Board of MAMTA-HIMC (MIRB/2022/007) on 10 August 2022. Written informed consent was obtained from all participants after explaining the purpose, procedures, duration, risks, and benefits of the study. Participants were assured of confidentiality in the case of publishing reports, articles, or conference abstracts, and were informed of their right to answer any questions or withdraw from the study at any time without prejudice.
Validation of the Tool
The research tool was validated for content validity by seeking opinions from thematic experts (n=3). Subsequently, after incorporating the suggestions and modifying the tool, it was subjected to pilot testing in the field to a tune of 21 respondents involving four outreach workers who were staff members of MAMTA. The tool was then titrated.
Figure 2: Key Contents of the Tool
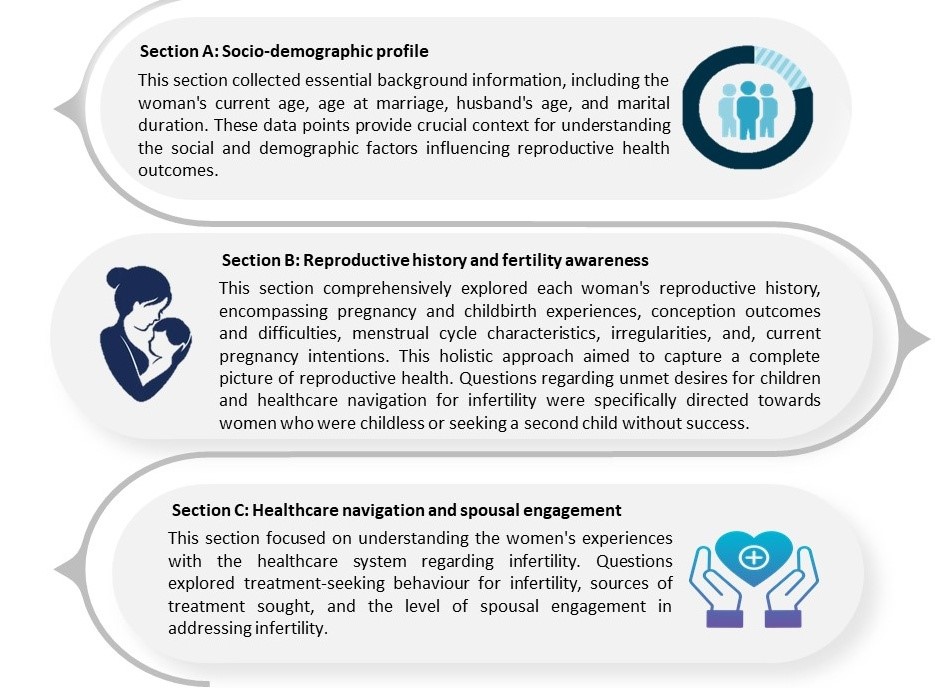
Source: Authors’ own
Selection of District for the Survey
Alwar district in Rajasthan was selected for this survey as its reproductive health profile was representative of the state. Alwar’s Total Fertility Rate (TFR) is at 2.8, as reported in the Annual Health Survey (2011–12), placing the district in the middle range compared to other districts in Rajasthan, where TFR values range from a high of 4.5 in Barmer to a low of 2.5 in Kota.
Alwar’s TFR reflects the reproductive health dynamics of a massive population of the state, making it a relevant site to study interventions aimed at addressing infertility and related reproductive health issues. Beneficiaries from this district are expected to represent broader health trends in Rajasthan, providing insights to inform reproductive health strategies across the state.
In addition, data from the National Family Health Survey-V (see Table 1) reveal several reproductive health challenges in Alwar, further justifying its selection for the study.
Table1: NFHS-V Indicators
| NFHS-V Indicators |
State |
District |
| Women ages 20-24 years married before the age 18 years |
25.4% |
32.24% |
| Women ages 15-19 years already mothers or pregnant at the time of survey |
3.7% |
8% |
| Women ages 15-24 yrs. who use hygienic methods of menstrual protection |
84.1% |
84.9% |
| Women ages 15-49 years who are anaemic |
54.7 |
53.3 |
Source: National Family Health Survey (NFHS-5), 2019-21[14]
The existing scenario in Alwar district, characterised by the prevalence of early marriage and pregnancy coupled with a significant prevalence of anaemia, creates a rationale for investigating infertility within the region. These interconnected factors can directly or indirectly contribute to infertility. Early marriage and pregnancy increase the risk of reproductive health complications, including anaemia, malnutrition, Sexually Transmitted Infections (STIs), and childbirth difficulties, all of which can contribute to future infertility. Anaemia, a significant public health concern in Alwar, can negatively impact reproductive health by disrupting the menstrual cycle, leading to irregular periods or the absence of menstruation. During pregnancy, anaemia increases the risk of miscarriage, premature birth, low birth weight, and maternal mortality.
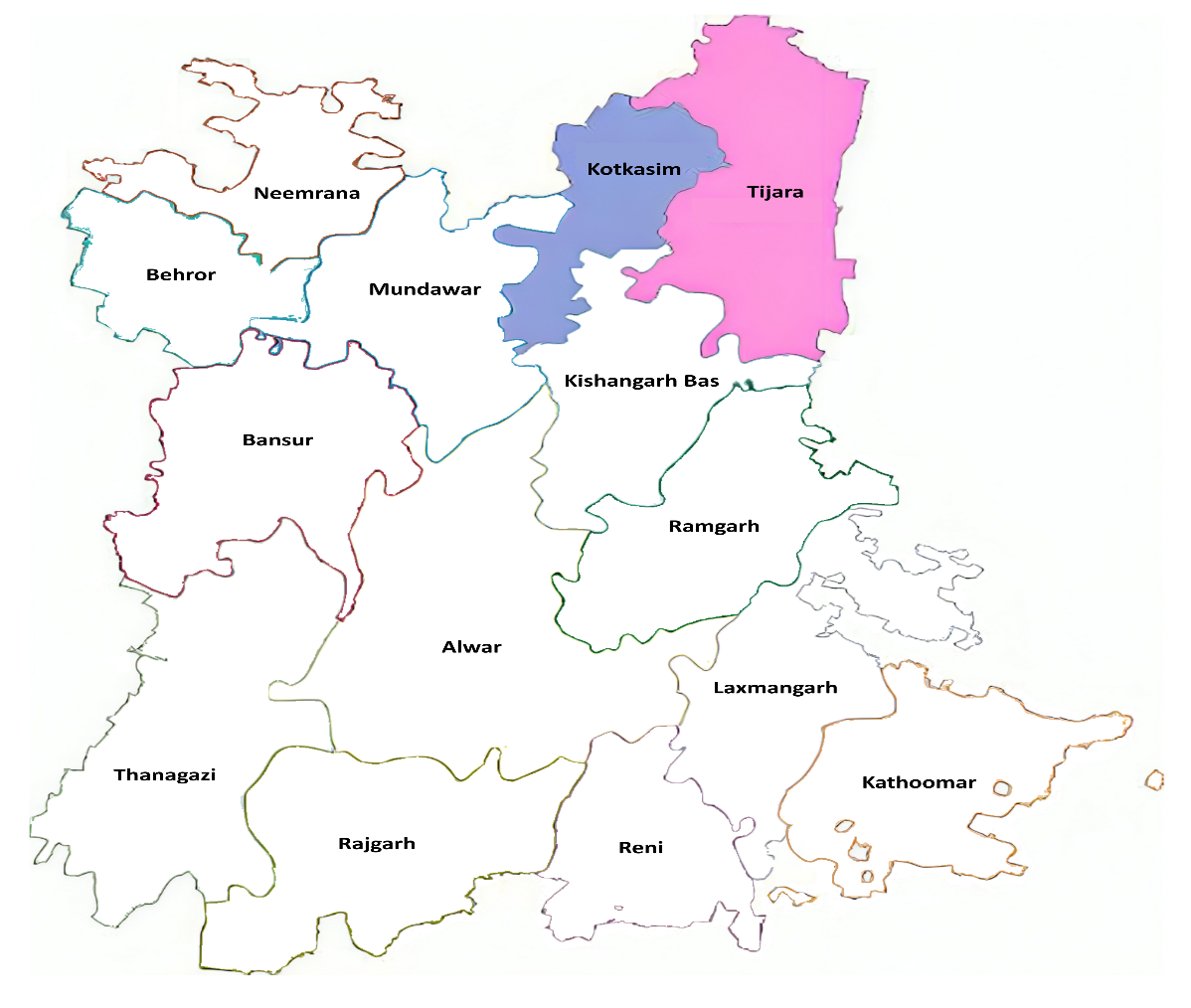
Block Selection for the Survey
The two blocks, Kotkasim and Tijara, were selected in consultation with the Alwar district administration. Engaging with the district administration from the outset fostered ownership and commitment, ensuring the long-term sustainability of the project and its potential integration into existing healthcare programmes. This participatory approach to site selection reflects best practices in community-based research, emphasising the importance of collaboration with local stakeholders to ensure the relevance and impact of research findings.
Community Engagement
The research team employed a multi-faceted, community-based approach to data collection, ensuring cultural sensitivity throughout the process.
Integrated Reproductive Health Assessment: Infertility-related questions were incorporated within a broader reproductive health assessment, minimising potential stigma[15] and providing insights into existing knowledge gaps and prevailing beliefs surrounding infertility.
“Most people in the community are generally unaware about the actual causes of infertility; they usually believe that either God is responsible or ghosts, etc. However, there could be many reasons, such as cysts in the uterus, excessive smoking, and drinking.” - ASHA worker from Baliyawas village
Empowerment of Local Women as Field Researchers: Local women, educated to at least the 12th grade, with some holding master's degrees, were trained in data collection and cultural sensitivity. This approach aligns with research emphasising the importance of local talent involvement in improving data quality and community relationships.[16]
Pre-survey Discussions: Village meetings and discussions with elders and community health workers were conducted to raise awareness about the survey's purpose and the importance of addressing infertility. These discussions also revealed the sociocultural importance of childbearing, as illustrated by a PRI member's statement about the societal pressures and traditional beliefs associated with having children.
"In our society, the main objective of marriage is to have children. Children are important because, when we grow cucumber or pumpkin, we keep the seeds—in a similar way, it is tradition and a need so that our own bloodline takes care of our property. Infertile couples have no one to bury their bodies when they are dead." - Panchayati Raj Institution (PRI) member from village Dumhera
Survey Implementation
Following these efforts, the survey commenced with married women of reproductive age. Consenting women provided information on their reproductive health history, fertility awareness, healthcare navigation practices, and spousal involvement in reproductive health matters.
Key Findings
Infertility Prevalence in Kotkasim and Tijara
The prevalence of infertility was calculated using the formula: Number of cases/total population surveyed x 100. In Kotkasim, out of 20,098 women surveyed, 350 were identified as suspected cases of infertility. In Tijara, 84 out of 6,262 women surveyed were suspected of infertility. This results in a suspected infertility prevalence of 1.75 percent in Kotkasim and 1.34 percent in Tijara.
Figure 3: Target Area
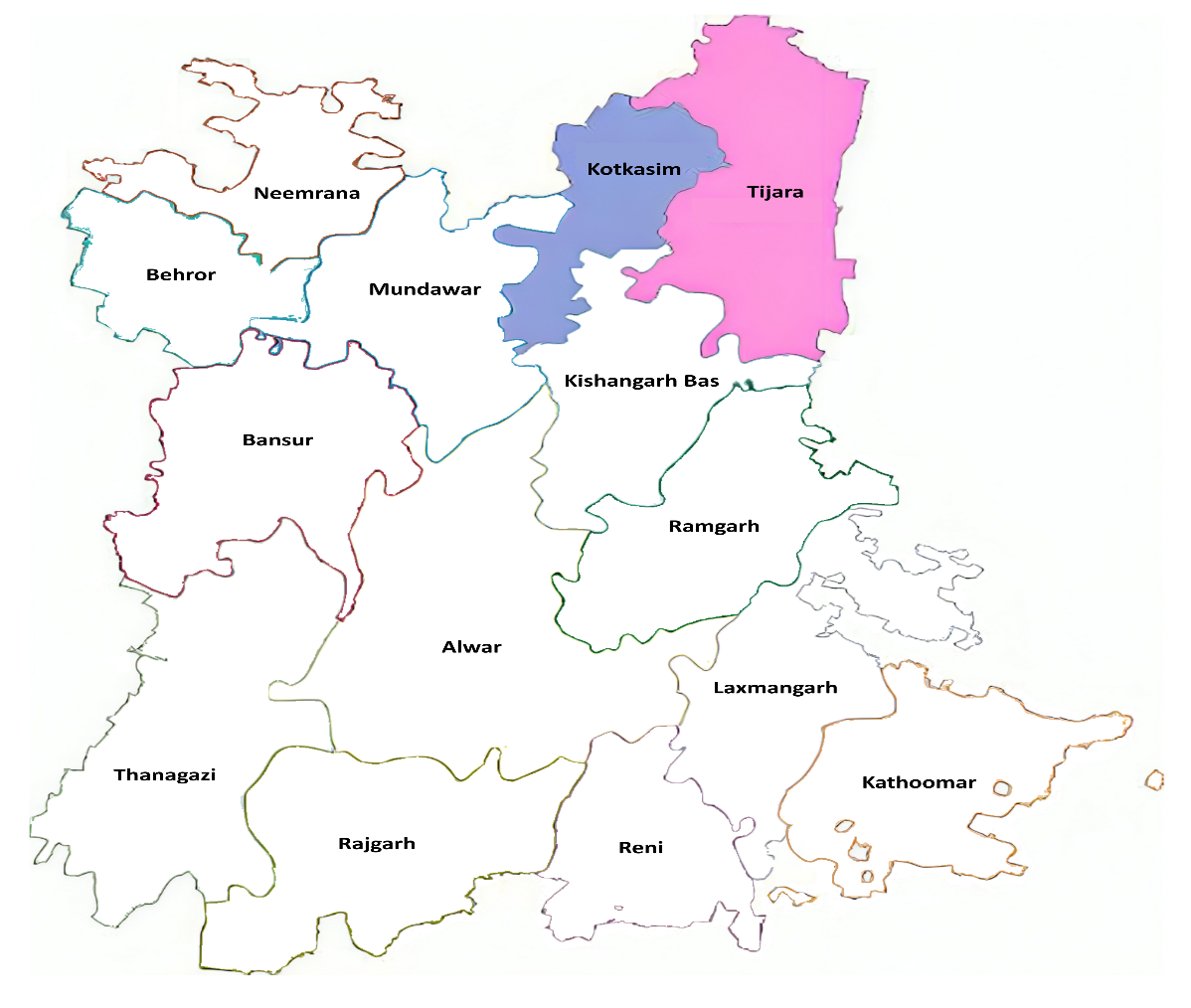
Source: Map created by authors. Base layer is free file from https://www.rajasthandirect.com/districts/alwar/map[17]
In Kotkasim, of the 350 women identified with infertility, 256 (73.1 percent) had primary infertility (no child and no history of conception), while 94 (26.9 percent) experienced secondary infertility (no child, but with a history of conception, including miscarriage or stillbirth). In Tijara, of the 84 women who experienced infertility, 65 (77.4 percent) had primary infertility, and 19 (22.6 percent) had secondary infertility. These findings provide insights into the prevalence and types of infertility within these communities, laying the groundwork for interventions and support services.
Potential Factors Linked to Infertility
Table 2 details the potential factors reported by the women suspected of infertility in the survey. One key finding was the high proportion of women (321 out of 434) who reported suspected infertility without a prior history of conception. This observation suggests several potential underlying factors:
Table 2: Reproductive History
| History of conception |
Kotkasim |
Tijara |
| Frequent miscarriages |
25 |
5 |
| History of miscarriage |
35 |
2 |
| History of still birth |
17 |
12 |
| Multiple pregnancies |
17 |
- |
| No such history |
256 |
65 |
| Total |
350 |
84 |
Source: Authors’ own
Undiagnosed Infertility: A substantial portion of these women may be experiencing undiagnosed infertility, characterised by underlying biological or physiological factors that impede conception. These factors could include hormonal imbalances, ovulatory disorders, or structural abnormalities in the reproductive system.
Male Factor: The survey relied on women’s self-reported data and excluded information on male factor infertility. The finding of ‘no history of conception’ suggests the possibility of male partner infertility, a factor that remains unaddressed in the current data.
Unexplained Infertility: Despite advances in reproductive medicine, a proportion of infertility cases remain unexplained, even after investigation. It is possible that some women in this study fall into this category, where no identifiable cause for infertility can be determined.
Underreporting and Recall Bias: The sensitive nature of infertility can lead to underreporting due to social stigma or fear of disclosure. Additionally, recall bias, where participants may not accurately remember or report past events, could also influence the data.
Discussion
Understanding infertility prevalence and the contributing factors is crucial for developing effective interventions. While India’s Assisted Reproductive Technology (Regulation) Act, 2021 regulates clinics, connecting women with the appropriate services remains a key policy challenge. Although an estimated 28 million couples experience infertility, only a small percentage pursue IVF.[18] This suggests that many infertility cases could be addressed through less intensive interventions.
Prioritising preventive measures and addressing underlying health issues in both men and women can help reduce the burden of infertility. Key interventions include expanding access to quality sexual and reproductive health services, encompassing screening and treatment for STIs and reproductive tract infections; addressing anaemia and promoting menstrual health; discouraging early marriage and pregnancy; enhancing delivery care; and raising public awareness about infertility risk factors. These interventions can address many infertility cases, reducing the need for complex and costly procedures like IVF.
A community-based approach could be key to identifying and supporting couples with suspected infertility. This should encompass a broad reproductive health assessment to understand the community context and minimise stigma. Infertility questions could be administered to sexually active, non-contracepting women who desire children and meet the criteria for primary and secondary infertility.
Engaging Accredited Social Health Activists (ASHA) in community-based identification and referral to appropriate health services can offer an immediate solution.[19] This report demonstrates that equipping ASHAs with tools can empower them to provide information and counselling on reproductive health issues, bridging the gap between community needs and health services.
With a training package based on the criteria defined earlier, ASHAs can provide initial support and counselling, effectively linking communities with appropriate healthcare services. By collaborating with community stakeholders, including village elders and gatekeepers, ASHAs can effectively meet the needs of couples suffering infertility.[20] Existing research in India supports the idea that ASHAs can effectively address couples’ needs through such collaborations.
Finally, integrating infertility treatment into the Jan Arogya Yojana, a key component of Pradhan Mantri Jan Aarogya Yojana (AB-PMJAY), could improve access to care. While research on integrating infertility care within India’s public health system remains limited, the Ayushman Bharat programme has shown promise in enhancing access to essential healthcare services.[21] Expanding its scope to encompass infertility care could address a critical coverage gap and alleviate the financial burden on individuals and couples seeking these services. This inclusion would align with the programme’s goal of universal health coverage and contribute to improved reproductive health outcomes nationwide.
Way Forward
With a budget of INR 110,062.14 lakh allocated for Reproductive and Child Health (RCH) services in 2025-26,[b] there is an opportunity to integrate infertility screening and basic counselling within the existing RMNCAH+N framework, leveraging existing infrastructure and personnel to reach couples experiencing infertility, particularly in rural areas. Further, the government can allocate a portion of the Health System Strengthening budget to train frontline workers on infertility-related issues, including basic diagnosis, counselling, and referral pathways for specialised care.
While a network of public and private healthcare facilities exists in Alwar district, such as Sawai Man Singh Hospital in Jaipur, Rajiv Gandhi Government General Hospital in Alwar, and district hospitals in Bhiwadi and Rewari, comprehensive infertility services within these facilities are absent. Furthermore, access to private hospitals like Solanki, Saniya, and Harish Hospital in Alwar may be limited by financial constraints. An understanding of existing solutions requires detailed information about the specific infertility-related services offered at each facility, including diagnostic tests, treatment options and associated costs. This landscape analysis of infertility services is essential for both individuals seeking care and policymakers aiming to improve access.
Endnotes
[a] National Family Health Survey V-2019-21;
chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/http://rchiips.org/nfhs/NFHS-5_FCTS/RJ/Alwar.pdf
[b] Information received from National Health Mission, Government of Rajasthan through personal communication on 8 January 2025.
[1] World Health Organization, Infertility Prevalence Estimates, 1990–2021, World Health Organization, 2023, https://www.who.int/publications/i/item/978920068315
[2] World Health Organization, “WHO Factsheet on Infertility,” May 2024, https://www.who.int/news-room/fact-sheets/detail/infertility
[3] World Health Organization, “1 in 6 People Globally Affected by Infertility: WHO,” April 2023, https://www.who.int/news/item/04-04-2023-1-in-6-people-globally-affected-by-infertility
[4] Mahey Reeta et al., “Fertility Awareness and Knowledge Among Indian Women Attending an Infertility Clinic: A Cross-Sectional Study,” BMC women's health 18 (2018): 1-7.
[5] Kumar Naina et al., “Impact of Age on Semen Parameters in Male Partners of Infertile Couples in a Rural Tertiary Care Center of Central India: A Cross-Sectional Study,” International Journal of Reproductive BioMedicine 15, no. 8 (2017): 497.
[6] “WHO Factsheet on Infertility”
[7] “WHO Factsheet on Infertility”
[8] “Infertility Prevalence Estimates, 1990–2021”
[9] Patrick John Rowe, “Clinical Aspects of Infertility and the Role of Health Care Services,” Reproductive Health Matters 7, no. 13 (1999): 103-111.
[10] Martha F. Davis and Khosla Rajat, “Infertility and Human Rights: A Jurisprudential Survey,” Columbia Journal of Gender and Law 40 (2020): 1.
[11] Chauhan Sanjay et al., “Capacity Assessment of District Health System in India on Services for Prevention and Management of Infertility,” Indian Journal of Community Medicine 43, no. 1 (2018): 19-23.
[12] Xiaochen Zhang et al., “Estimating the Effects of Policies on Infertility Prevalence Worldwide,” BMC Public Health 22, no. 1 (2022): 1378.
[13] Deborah S. Carr and Halvorsen Kathleen, “An Evaluation of Three Democratic, Community-Based Approaches to Citizen Participation: Surveys, Conversations with Community Groups, and Community Dinners,” Society & Natural Resources 14, no. 2 (2001): 107-126.
[14] International Institute for Population Sciences (IIPS) and ICF, India Districts Factsheet National Family Health Survey (NFHS-5), 2019-21 (Volume II), Mumbai, IIPS.
[15] McDavitt Bryce et al., “Peer Reviewed: Dissemination as Dialogue: Building Trust and Sharing Research Findings Through Community Engagement,” Preventing Chronic Disease 13 (2016): E38.
[16] Derose Kathryn Pitkin et al., “Learning About Urban Congregations and HIV/AIDS: Community-Based Foundations for Developing Congregational Health Interventions,” Journal of Urban Health 87 (2010): 617-630.
[17] “District Map of Alwar,” https://www.rajasthandirect.com/districts/alwar/map
[18] PRS Legislative Research, “Assisted Reproductive Technology (Regulation) Bill, 2021,” 2021, https://prsindia.org/files/bills_acts/bills_parliament/2020/Issues%20for%20Consideration%20-%20ART%20Bill,%202021.pdf
[19] Sumitra Dhal Samanta et al., “Examining the Feasibility and Acceptability of Mobile Based Interactive 4 Voice Response System for Delivering Reproductive Health Messages in Rural India," Journal of Women's Health, Issues and Care 10, no. 7 (2021): 1-5.
[20] Pankhuri Sharma et al., “Effectiveness of Community Intervention Program to Improve Maternal Healthcare Services Uptake Among Young Married Women in Rural India,” Journal of Women’s Health Care 7, no. 3 (2018): 2167-0420
[21] Grewal Harpreet et al., “Universal Health Care System in India: An In-Depth Examination of the Ayushman Bharat Initiative,” Cureus 15, no. 6 (2023): e40733.
The views expressed above belong to the author(s). ORF research and analyses now available on Telegram! Click here to access our curated content — blogs, longforms and interviews.

 PDF Download
PDF Download


 PREV
PREV


